



|
A Bayesian Modelling of Malaria in the South of Iran: The Effect of Socio-demographic Factors |
|
Amin Ghanbarnejad1, Habibollah Turki2, Mehdi Yaseri1, Ahmad Raeisi 3,4, Abbas Rahimi Foroushani 1* |
|
|
|
1 Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. 2 Infectious and Tropical Diseases Research Center, Hormozgan Health Institute, Hormozgan University of Medical Sciences, Bandar Abbas, Iran. 3 Departments of Medical Parasitology and Mycology, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. 4 Center for Communicable Diseases Control, Ministry of Health and Medical Education, Tehran, Iran. |
ABSTRACT
Background: Malaria threatens about 40% of the world population. WHO designed programs for eliminating malaria. The malaria elimination program has been running since 2010 in Iran. The success of this program is related to determining its determinants especially socio-demographic factors. The main goal was to investigate the association between socio-demographic factors at the county level with the incidence of malaria in Hormozgan Province counties during 2011-2017.
Methods: The data consists of 882 confirmed cases gathered from the Communicable Disease Center (CDC) in the Health Deputy of Hormozgan University of Medical Sciences. A Bayesian Poisson model was used for modeling the data. All analyses were done in R studio and WINBUGS software.
Results: The Incidence Ratio for malaria ranged from 0 (Abu Musa and Haji Abad districts) to 280.57 (Bandar–e-Jask). Based on model, urbanity (RR=0.76; 95% credible interval: (0.65, 0.96)) and Health Center Density (RR=0.98; 95% credible interval: (0.96, 0.99)) had negative effect on malaria incidence, but children under 6 years (RR=1.65; 95% credible interval: (1.07, 2.50)), foreign immigration (RR=1.14; 95% credible interval: (1.11, 1.17)) and illiteracy (RR=1.12; 95% credible interval: (1.10, 1.15)) had incremental impact.
Conclusion: It was found that the social-demographic factors such as illiteracy, urbanity, children population, and managerial factors such as Health Center Density and also population mobility play an important role in malaria transmission. Therefore, the malaria surveillance system should continue to be vigorous in the region, especially in the low income or low educated regions.
Key Words: Bayesian, Poisson, Malaria, Socio-demographic, Immigrants, Urbanization.
Malaria is one of the tenth diseases under investigation by the WHO as part of a program, called Tropical Disease Research. About 40% of the world's population is at risk of malaria which is estimated to be about 2.5 billion people worldwide. According to the report by WHO in 2019, about 80 countries are facing malaria transmission which had led to 228 million infected cases and 405,000 death [1].
The disease is present in most tropical, subtropical, and even temperate regions of the world. It is not possible to solve the disease problem with a single strategy. Malaria is not only infectious disease in tropical areas but also a health problem related to social-demographic characteristics, economic, and developmental conditions in the world [2]. This disease also affects the quality of life of patients and it is more vulnerable in children [3]. Some studies showed that wealth and managerial inequality in the regions can result in a different burden of Malaria morbidity [4].
Iran is located in an endemic area of malaria according to malaria's global distribution map. Although ongoing efforts to combat malaria in the last five decades have led to a significant reduction in malaria in Iran, there are still positive cases of malaria, especially in the south and south-east of the country [5]. Hormozgan Province in the south of Iran is one of the districts which is dealing with malaria elimination program [6, 7]. Approximately 10% of cases reported in Iran and about 12% of malaria cases in the south-eastern region are owned by this province [5, 8].
WHO designed an elimination program for some countries such as Iran to combat Malaria in them. The first phase of implementation in Iran was begun from 2010 to 2015, and the health policymakers continue the program in the region [9-13].
Hormozgan is one of the five poorest provinces of Iran [14, 15] and there is a low practice about malaria transmission and control methods in some areas [16]. Relocation and presence of immigrants infected with malaria, especially Pakistani and Afghan are of the factors affecting the malaria situation in this province [10, 11].
Since we are interested to evaluate the association between the covariates at the county-level with the burden of a disease, the best classes of models are Poisson models. These models are widely used in the modeling of malaria [17-19]. To the best of our knowledge, no previously published study has assessed the socio-demographic factors at the county level and incidence of malaria in Hormozgan province, south of Iran.
The main goal of the present study was the investigation between socio-demographic factors at administrative districts, namely county with the risk of malaria in a region previously was categorized as an endemic area for malaria infection and the elimination program that is implemented in the region.
MATERIAL AND METHODS
Study Area
Iran is in the endemic area of the global malaria distribution map [2]. Most of the positive cases are in the south and south-east of the country, where the malaria elimination program is in progress. The three provinces of Kerman, Sistan, and Baluchestan, and Hormozgan are malaria-prone areas of Iran. Hormozgan is one of the malaria-prone areas of the country and has been hyper-endemic for many years [5]. This province is located in the south of Iran, with about 1,000 km of coastline. Its population was 1,578,183 based on 2016 census data [20]. Its area is 70,697 km2 and its provincial capital is Bandar Abbas. The location of the study area is shown in Figure 1.
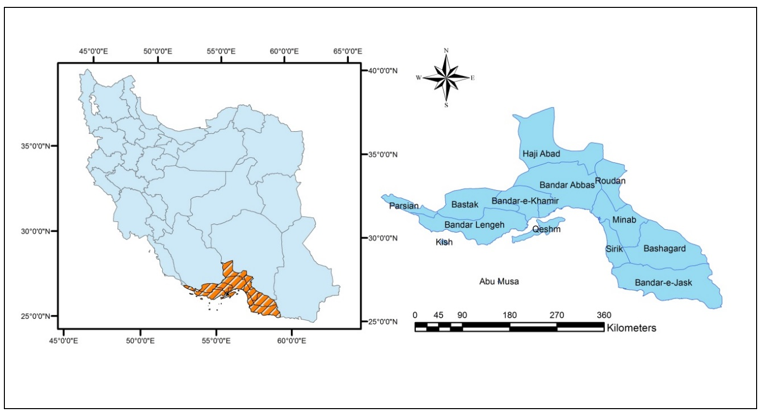
Figure 1. Location of the study area, Hormozgan province, Iran
Data Collection and Covariates
The data on malaria incidence from 2011 to 2017 in Hormozgan province was used for analysis. This data was collected from the Communicable Disease Center (CDC) in Health Deputy of Hormozgan University of medical sciences, located in Hormozgan province, Bandar Abbas city. The data on the number of malaria cases were available at the county level. The data on socio-demographic variables were gathered from the Statistical Department in Deputy of Health and Iranian Statistical Center [20].
The socio-demographic variables included in this study were available at the county level: illiteracy, foreign immigration, urbanity, age below 6, health center density, and population density. Illiteracy was defined as the percentage of persons who were 6 years old and older that did not go to school at all. Foreign immigration was defined as the percentage of foreigners who lived in each county. We defined urbanity as the percentage of people who lived in an urban area and categorized this variable into two groups with a cut-point of 50%. The covariate age below 6 was measured as the percentage of the children who were 6 years old and younger in the whole population and defined as a dichotomous variable with two groups: less than 10% and equal or greater than 10%. Health center density was defined as the number of health center per 100,000 population of each district. The population density was calculated as the number of persons who lived in 1 square kilometer of the region.
Statistical Model
For the response variable, we analyzed the observed numbers yi of malaria cases (i: county (1,…,14)). The model used in this paper was a Poisson model with illiteracy, foreign immigration, urbanity, age below 6, health center density, and population density as covariates. The following Bayesian structure was considered for the modeling:
of malaria cases (i: county (1,…,14)). The model used in this paper was a Poisson model with illiteracy, foreign immigration, urbanity, age below 6, health center density, and population density as covariates. The following Bayesian structure was considered for the modeling:
We used the population of each county as an offset and added it as a logarithmic form to the model formula. The β=β1,…,βj, j=1,…,6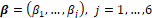 is the vector of coefficients and the xi
is the vector of coefficients and the xi is a vector of covariates for the ith region. For βj
is a vector of covariates for the ith region. For βj , we considered a Normal distribution with a mean of 0 and a precision parameter of 0.001 as prior.
, we considered a Normal distribution with a mean of 0 and a precision parameter of 0.001 as prior.
RESULTS
Descriptive Statistics
The study included 882 registered cases in the period from 2011 to 2017. Based on epidemiological classifications, 716 cases (81.2%) were imported. The high portion of imported malaria led us to investigate the effect of foreign immigration on the incidence of Malaria in the study region. The data was available at the county level for model fitting. The 7-year incidence ratio of malaria per 100,000 persons was calculated as the number of cases in each county divided by its population multiplied by 100,000, which is shown in Figure 2. The incidence ratios ranged from 0 (Abu Musa and Haji Abad county) to 280.57 (Bandar–e-Jask).
Figure 2. The Incidence Ratio of Malaria in South of Iran, Hormozgan Province
The descriptive statistics of covariates are presented in Table 1. As mentioned in Table 1, 4 regions had urban residency above 50%. Only in one county, children below 6 years were less than 10% of the total population. On average, 3% of the population was foreign immigrants, but they were responsible for about 80% of Malaria cases. About 99 persons lived in each square kilometer of the region. Although the variation of population density was high because of the large values associated with two islands of Hormozgan, there were about 14 Main Health Centers per every 100,000 population. There were 194 Main Health Centers in Hormozgan. On average, about 10% of people were illiterate.
Table 1. Summary of Statistics for Socio-demographic Covariates
|
Variable |
Categorical Covariates |
Quantitative Covariates |
||
|
Categories |
No. (%) |
Mean ± SD |
Range (Min-Max) |
|
|
Urbanity |
< 50% |
10 (71.43%) |
|
|
|
≥ 50% |
4 (28.57%) |
|
|
|
|
Children below 6 Years |
<10% |
1 (7.14%) |
|
|
|
≥ 10% |
13 (92.86%) |
|
|
|
|
Foreign Immigration (%) |
|
|
3.10 ± 3.57 |
0 – 13.29 |
|
Population Density (per km2) |
|
|
99.27 ± 174.83 |
3.77 – 553.97 |
|
Health Center Density (per 100,000 Persons) |
|
|
14.38 ± 6.56 |
4.84 – 28.57 |
|
Illiteracy (%) |
|
|
10.24 ± 5.64 |
0.30 – 21.75 |
Model Fitting
The Bayesian Poisson model was fitted to the data through MCMC and Gibbs sampling method with 50000 iterations after burning of the first 10000 iterations. We set thinning parameter to 5 to reduce the autocorrelation. The regression coefficients and risk ratio of covariates influence malaria incidence with the 95% Bayesian credible intervals that are reported in Table 2.
Table 2. Summary Statistics of the Coefficients of Bayesian Poisson Model for Malaria Incidence
|
Variable |
Categories |
Regression Coefficients |
95 % Credible Interval for Regression Coefficients |
Risk Ratio |
95 % Credible Interval for Risk Ratio |
|
Urbanity |
< 50% |
|
|
1 |
|
|
≥ 50% |
-0.227 |
(-0.436 , -0.037) |
0.758 |
(0.647 , 0.964) |
|
|
Children below 6 Years |
<10% |
|
|
1 |
|
|
≥ 10% |
0.501 |
(0.068 , 0.918) |
1.650 |
(1.070 , 2.504) |
|
|
Foreign Immigration (%) |
|
0.127 |
(0.101 , 0.153) |
1.135 |
(1.106 , 1.165) |
|
Population Density (per km2) |
|
-0.0008 |
(-0.0028 , 0.0009) |
0.9992 |
(0.9972 , 1.0009) |
|
Health Center Density (per 100,000 Persons) |
|
-0.024 |
(-0.046 , -0.001) |
0.976 |
(0.955 , 0.999) |
|
Illiteracy (%) |
|
0.116 |
(0.093 , 0.138) |
1.123 |
(1.097 , 1.148) |
As mentioned in Table 2, the effects of foreign immigrants, illiteracy, and children below 6 years on malaria incidence were positive although urbanity and Health Center Density had a negative impact on malaria incidence. All the above covariates were significant at 5% level because the Bayesian credible interval did not include the null value of 1 in terms of Risk Ratio. Also, the effect of population density was not significant at the 5% level.
As seen in Table 2, the risk of malaria in regions that had at least 50% of urbanity was 24% less in comparison with regions with urbanity less than 50%. The risk of malaria was increased by 65% in regions that had children below 6 years of 10% or greater in their population pyramid. With every 1 percent increase of foreign immigrants, the risk of malaria was increased by 13.5%. Increasing one Health Center per 100,000 persons was associated with a 2.4% decrease in malaria risk. The malaria risk was increased by 12.3% with every one percent increase of illiteracy in the region.
DISCUSSION:
In this study, the relationship between malaria incidence and socio-demographic factors at the county level was assessed based on the Bayesian Poisson model in Hormozgan province at the county level. Determining social and demographic covariates associated with malaria at the administrative level can help health policymakers to have a better road map for intervention and eradication of the disease. The social and demographic factors are more feasible to intervene than climate factors because the climate determinants are not in our hands.
The Bayesian framework was used for modeling the malaria incidence after adjusting for socio-demographic variables: illiteracy, foreign immigration, urbanity, age below 6, health center density, and population density. This is the first research that used a Bayesian modeling framework to study the relationship between socio-demographic covariates and malaria infection in Hormozgan province at the administrative level.
Based on Bayesian modeling, urbanity was an important covariate on malaria. In the region with 50 percent and more degree of urbanization, the risk of malaria was estimated to decrease by 24% approximately. This can be explained by the association of urbanity and developmental factors such as electricity and access to healthier water. This result is consistent with the study by Flückiger et al in China; they concluded that urbanization and economic activity have resulted in decreasing malaria [21]. Kabaria et al. investigated the effect of urbanization and they concluded that the risk of malaria infection was declined from rural areas through to urban areas [22]. They found a significant and important effect of population density, however, in this study, there was no significant effect of population density. Finda et al. concluded that the dramatic decline of malaria in south-eastern Tanzania could be associated with urbanization and improved housing [23] which is following our study. In another study in northwest Acre, Dal’Asta et al. found that the role of urbanization on malaria is important and it is necessary to have different programs for urban and rural settlements [24]. Feged-Rivadeneira et al showed in the study in Peru that living in pre-urban areas in comparison with living in forested areas, leads to a decrease the malaria infection. They also found a significant and negative impact on population density [25]. Although the population density was not a significant factor in our study, we emphasize the negative effect of this covariate on malaria incidence.
We found that when the children below six years form more than 10% of the population, we should be expecting an increase of 65% in malaria risk in the region. We can interpret this result because the children are more vulnerable to diseases especially infectious diseases such as malaria [26]. Ndiaye et al. in Senegal proposed that the treatment for age under 5 years must be different [27]. Cohee et al. performed a review article and found that areas with more children are more risky in terms of fatality and morbidity of malaria [28].
We found that foreign immigrants play an important role in malaria transmission in Hormozgan. The majority of immigrants were from Afghanistan and Pakistan and they are workers. Early detection of malaria in this group can result in a significant reduction of disease burden. Opie et al. concluded that foreign immigrants infected with malaria are imposing a significant burden on health resources [29] which is following our study. Chen et al. investigated the effect of population mobility in the China-Myanmar border region of Yunnan Province, China on malaria incidence. They found that a high number of moveming population was linked with greater malaria susceptibility [30].
Another finding of the present study was the negative impact of illiteracy on malaria incidence. As shown in the result section, one percent increase in illiteracy in the districts was linked to an increase of the malaria risk by about 12%. Education is associated with better knowledge about transmission and practice of preventing tools such as ITN. Nyadanu et al. conducted a study in Ghana to investigate the relationship between having basic education and malaria incidence and they found a positive strong correlation between basic education and malaria incidence which is in line with our study [31]. Canelas et al. found that in Brazilian Amazon, illiteracy results in a 10% increase in malaria transmission [32]. Ozougwu conducted a study among children in Nigeria and concluded that malaria infection is lower in educated areas [33] which confirms our findings.
Health center density was a health management index which is affected malaria in the region. This index represents the capability of the health network for covering the population and gives them the health services they need. This index was significant and we concluded that with increasing one health center per 100,000 persons, we expect to decrease the malaria risk by 2.4%. In a study by Ssempiira et al. in Uganda, the mortality rate of malaria decreased by increasing the health facility readiness [34].
CONCLUSION:
Based on the analysis of the study results, it was found that the social-demographic factors such as illiteracy, urbanity, children population, and managerial factors such as Health Center Density and also population displacement play important role in malaria transmission. Inequality of the factors across counties, lead us to think about different programs for different counties to achieve a good plan for controlling and eradication malaria. Therefore, the malaria surveillance system should continue to be vigorous in the region, especially in the low income or low educated regions.
ACKNOWLEDGMENTS
The authors would like to express gratitude to the staff of the Communicable Disease Center of Hormozgan University of Medical Sciences especially Mr. Sajjad Fekri for gathering the data. We are also glad to thank the other staff of the Deputy of Health of Hormozgan University of medical sciences. This research is part of a Ph.D. Thesis in Biostatistics funded by Tehran University of Medical Sciences.
Conflict of Interest
There is no conflict of interest.
REFERENCES